She’s spent years focusing on therapy that supports personal healing. Now, Katarina Svabcikova is introducing these techniques to patients at IU Health Simon Cancer Center.
By IU Health Senior Journalist, TJ Banes, tfender1@iuhealth.org
She is no stranger to the hospital setting. Katarina Svabcikova supported a mindfulness intervention program to help nurses and physicians manage the stress related to COVID-19.
More recently, she joined IU Health’s Center for Mindful Practice as a Yoga Teacher and a Wellness Consultant focusing on how mindfulness practices help release stress and tension in the body.
When she had an opportunity to join IU Health Simon Cancer Center, she already knew the benefits of yoga as part of holistic healing. Svabcikova starts the New Year with a goal of showing patients the simplicity of breathing and the benefits of following well-crafted mindfulness practices.
Yoga is part of the CompleteLife Program of the Cancer Resource Center at IU Health Simon Cancer Center. Other therapies – including art, massage, and music – are offered as a way of attending to the mind, body, and spirit of patients. Support groups and other resources are also part of the Cancer Resource Center located on the first floor of Simon Cancer Center.
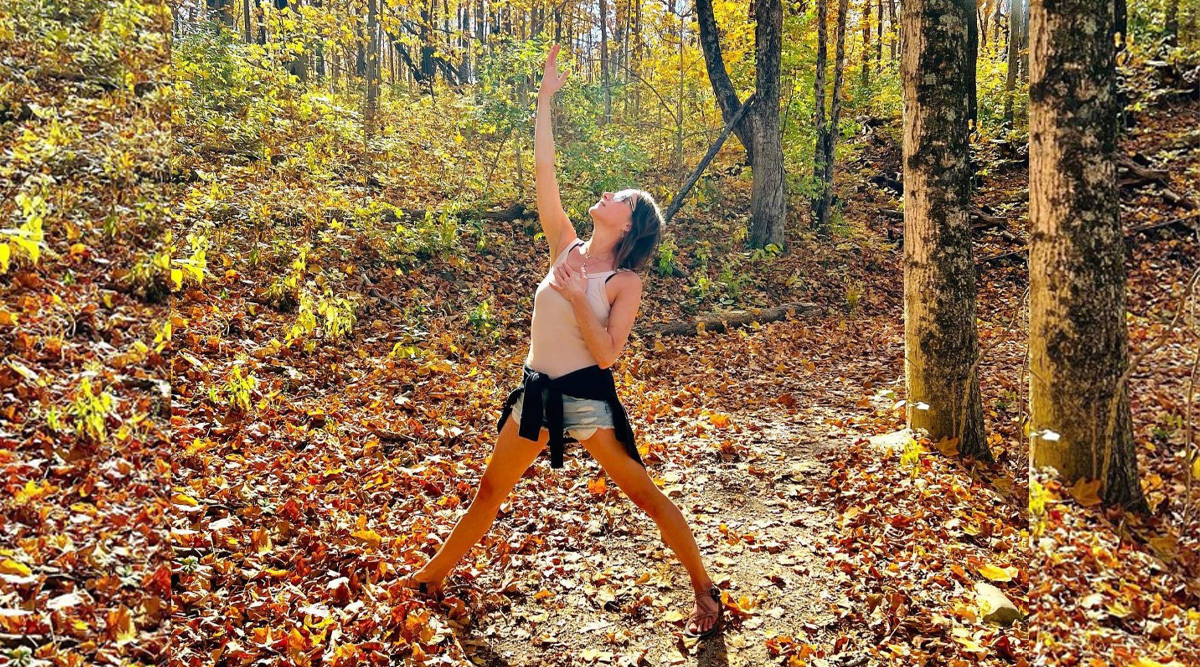
Svabcikova is originally from Slovakia and first came to the United States as part of a Master of Business Administration program. She returned later and has lived here for the past 16 years. She has practiced yoga for the past 10 years. She has been a guest teacher at various trainings, and was a co-leader of 2019 Monumental Yoga.
After experiencing a traumatic event in 2015, Svabcikova says yoga saved her life. “Through my own experience of trauma I have been led to passionately study the topic of healing, trauma, PTSD, vagus nerve regulation, neuroscience, as well as practices to deepen my trust, compassion, forgiveness, and grace as a way of healing myself,” she said.
“I have been fascinated by the healing journey involving the nervous system in general and I became absorbed in how we can combine yoga practice with science-based understanding of the body and mind to regulate the nervous system,” said Svabcikova. She also works with clients at the Indianapolis Trauma Therapy Center.
Teaching and guiding patients, she said is one of the most joyful activities of her life. “Through my teaching I encourage students to be the best versions of the themselves, because everything we need to know is already in us.”
With a focus on oncology patients, Svabcikova meets them where they are – whether they are resting in their bed or sitting in a chair. She gently coaches them through exercises that promote mindfulness. The practice is also beneficial to family members navigating a diagnosis of a loved one.
One family member recently expressed how she felt anxious knowing her loved one was about to be discharged. She worried if she could care for him. She had observed Svabcikova working with her loved one and she too began to practice the technique.
“A cancer diagnosis can take the cancer patient’s breath away and yoga can give it back,” said Svabcikova. “Treatments can be counterintuitive to mindfulness so I want to introduce them to a simple easy-to-follow practice. The breath is available to all of us – even if they are in fight or flight mode or freeze mode. Breath can soften the mind and give them a little reprieve from stress and fear.”