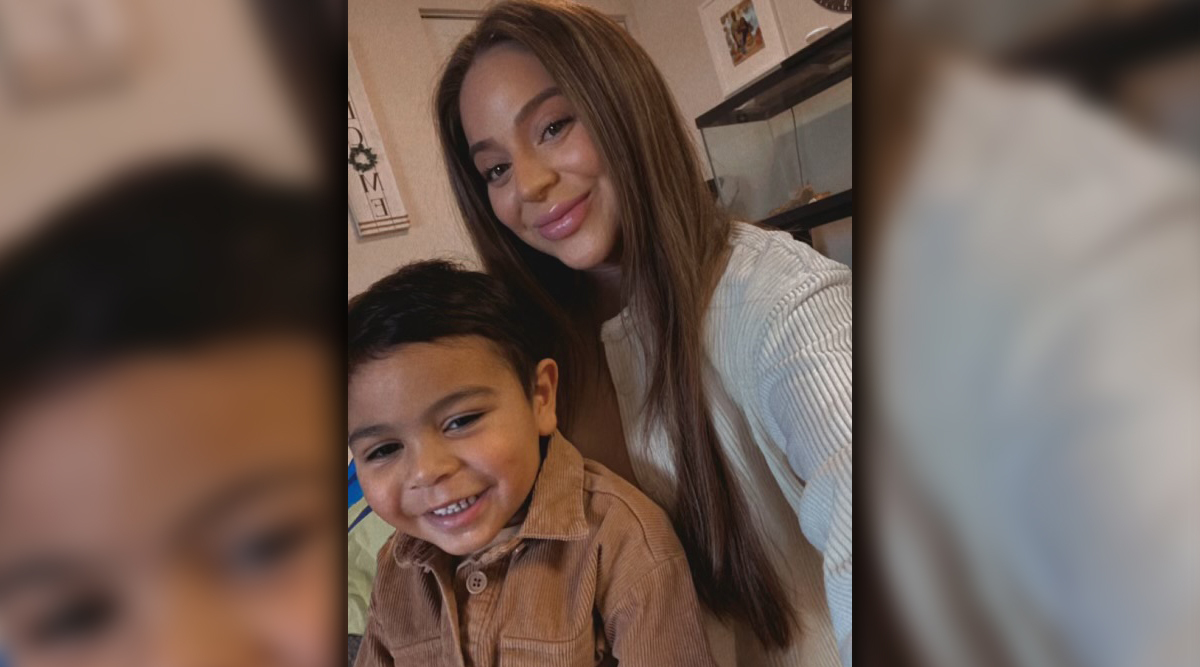
Her mother describes her as “upbeat.” Karina Ontiveros has been through more than many 24-year-olds.
By TJ Banes, IU Health Senior Journalist, tfender1@iuhealth.org
She had been working out and lost 50 pounds. Karina Ontiveros wasn’t overly concerned when she had some back pain. But when it began traveling up her neck, she thought something must be wrong.
Then she doubled over in pain.
“I thought I was having a heart attack. My arm was tingly and the pain was sharp,” said Ontiveros. At the time she was 23. She was working as a bartender, helping with her family’s restaurant, a wedding planner, and raising a toddler.
She saw three doctors and had three x-rays at healthcare centers near her Portage, Ind. home. She was given muscle relaxers and steroids and told to go home and relax. When she got a cough, she was told it was a side effect of the steroids. Ontiveros never took the muscle relaxers. She didn’t have a good feeling about them.
After her third x-ray she left thinking everything was fine. A few hours later she received a call from the urgent care doctor telling her to go to the ER immediately and ask for a CT scan.
“I waited a little because I had to settle this in my mind what was actually happening,” said Ontiveros. She went alone to the hospital, even though her fiancé had offered to accompany her.
“I honestly just thought I’d go in and they’d say everything is fine because I already had x-rays,” said Ontiveros. An hour later she learned she had a tumor behind her sternum. It had been hiding in previous x-rays. It was Dec. 16, 2023. She was transferred to a bigger nearby hospital for a biopsy and then waited.
Doctors initially described her cancer as a germ cell tumor. They referred her to IU Health Simon Cancer Center where Dr. Lawrence Einhorn specializes in germ cell tumors. She was in the hospital for three days and also underwent genetic testing. Her results wouldn’t be back for a few days so they sent her home for Christmas. Two days after Christmas she found she was pregnant and also had non-Hodgkins lymphoma, not a germ cell tumor.
Non-Hodgkins lymphoma starts in the lymphatic system, part of the body’s germ-fighting immune system.
“I had been trying to get pregnant for a year and had started taking progesterone pills. With everything going on, it hadn’t hit me that I hadn’t started my period,” said Ontiveros. “When I was in the hospital, I found out I had cancer and I was also pregnant. I was worried. I had already a CT scan with dye and a biopsy with other medications.”
With her new diagnosis, Ontiveros began her care with IU Health’s Dr. Rita Assi who specializes in cancer treatment at the IU Simon Cancer Center Hematology Clinic. She also has experience with women who are pregnant or trying to get pregnant.
“They said I had an excessive amount of fluid around my heart that needed to be drained before I could begin chemotherapy the beginning of January. They drained 50 millimeters and sent me home with a drain. Another 50 millimeters were drained and she returned to IU Health to begin treatment.
“I got an ultrasound, there was a heartbeat and they decided I was six weeks along. I couldn’t start chemo until I was 12 weeks pregnant,” said Ontiveros. “I wanted to get through this and there was no way I was going to have an abortion.” Not long after the ultrasound, Ontiveros miscarried the pregnancy.
She met with a fertility specialist at Riley Hospital and talked of freezing eggs; she looked at all options. “Dr. Assi was the sweetest. She knew my whole story and she has given me confidence that I can get pregnant again,” said Ontiveros.

She started chemotherapy the first week in February and will complete six cycles.
“At one point I wanted to be a doctor and now I’m seriously considering going back to school for nursing. The nurses here have been so supportive to me,” said Ontiveros.
“I feel like she’s been so positive through all of this. She speaks up for herself and is stronger than you can imagine,” said her mother, Angela Mendoza.

