When
Sharon Hollis realized she was addicted to alcohol, she sought help from IU
Health West’s Addiction Treatment and Recovery Center. Now, she hopes to help
others by sharing her journey.
By Emma
Avila, epackard1@iuhealth.org, writer
for IU Health’s Indianapolis Suburban Region
For Sharon
Hollis, her drinking started gradually. It was a drink socially, then a drink
alone, then stronger drinks and then hard liquor. It happened over about a year
and took her some time to realize she needed help.
“I had no
idea what a slippery slope I was on. I had no idea I had become addicted,” she
said.
She used
alcohol to help combat sadness and stress, with the COVID-19 pandemic playing a
large role. She realized if she didn’t drink, she would experience tremors.
Even then, it was difficult to reach out and ask for help, but Hollis knew she
had to do what was best for herself.
“I was
ashamed to reach out. This isn’t who I am. I was afraid it would tarnish my
business,” she said.
Asking
for help
She reached
out to a friend, who happened to be a physician at IU Health West. Through that
connection, she was met Marlene Villecco, an addiction counselor at the IU
Health West Addiction Treatment and Recovery Center (ATRC).
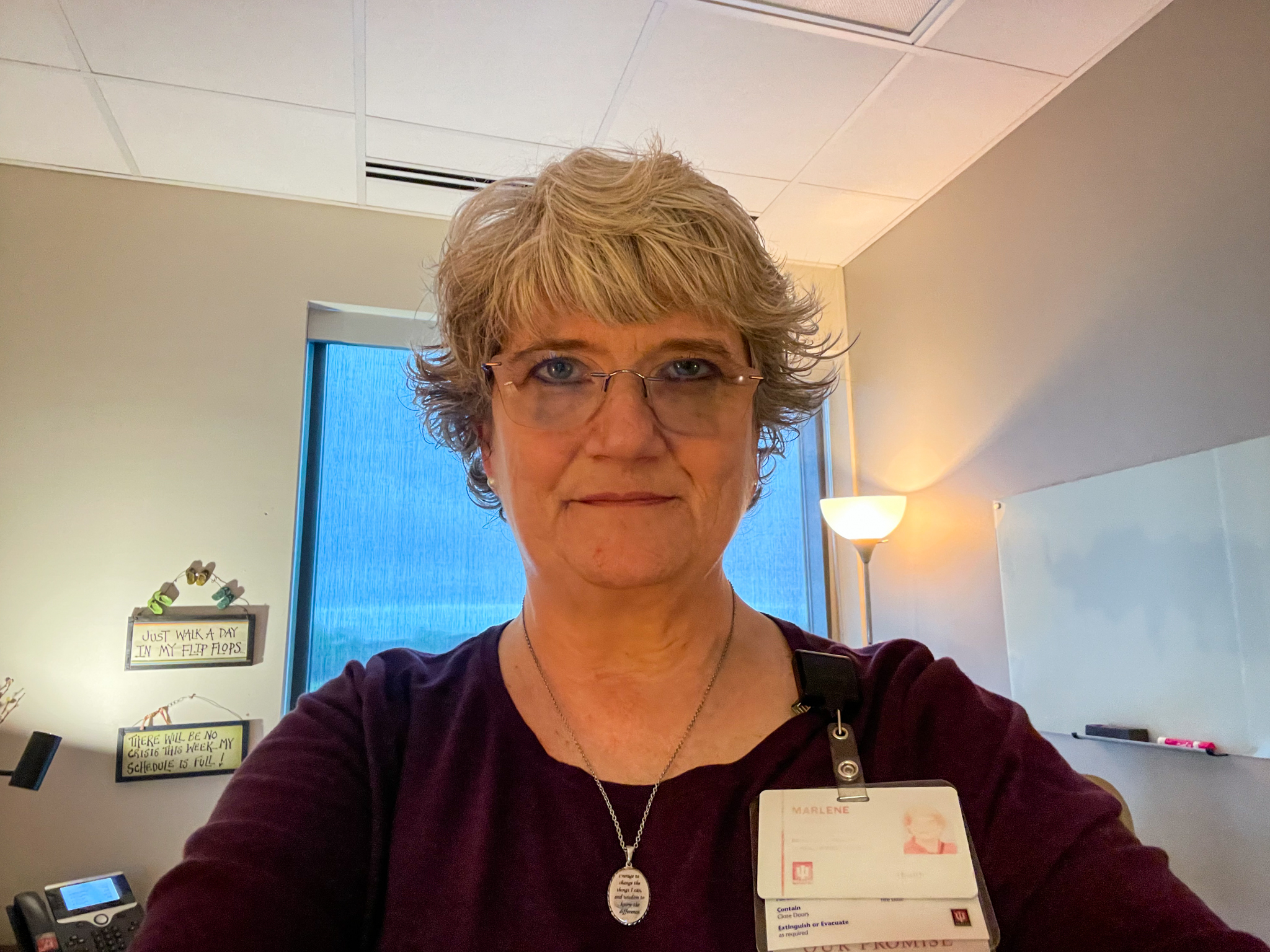
She started
on a six-week program just days later. She met with Villecco once a week and
attended group counseling every night.
“The
standard amount of time someone who is recommended to our substance use
disorder (SUD) program here is anywhere from six to eight weeks, based
upon the patient’s needs,” Villecco explained. “Every patient is different, so
there is no set cookie cutter way of treatment for everyone that enters our
program.”
Hollis found
counseling beneficial. She learned what her triggers were and developed new
coping skills.
“The biggest
part that stuck out and has stayed with me is I could not believe how poor my
coping skills were until I got into group,” she said. “It helped me understand
myself. I use the coping skillset I learned in my business. I use them in my
personal daily life.”
“Our
evidence-based curriculum is set up to help educate, teach and discuss topics.
This includes early challenges in recovery, how to work through and process
emotions again, how to better communicate, setting and maintaining strong
boundaries with family and friends as well as how to develop healthy
relationship that will support their recovery,” Villecco added. “The final goal
is helping them to develop a relapse prevention plan that is going to support
their recovery.”
The road
to recovery
Hollis
learned new things about addiction, and the information helped eliminate some
former biases she had surrounding substance use.
“Addiction
in general, I am guilty of not understanding it. After I got started in
treatment, my compassion for people with addictions of all kinds has expanded,”
she said. “What I learned was that this disease, this problem, affects everyone
across the board.”
During her
recovery, Hollis took a step back and saw how her addiction hurt herself and
those around her. It had a deep impact on her wife and adult son.
“I wish I
would’ve known when I was drinking that I needed to be still and not make
compulsive decisions. Because I was doing that, I hurt everyone, including my
spouse,” she recalled. “Some people say alcohol is a truth serum. For me, it
made it easy to lie because I didn’t want to expose my issues. The lying
damaged my integrity, both to myself and to others. That is not who I am.”
After
completing her six-week program, Hollis continues to go to the occasional
meeting, if she feels it is necessary. Villecco was glad Hollis has been so
open to the program and recovery as a whole.
“I will have
to say, Sharon has been one of those patients that everyone loves to work with.
She is someone who has the willingness to keep an open mind to learn and
practice new tools that will help with her recovery management,” Villecco
said.
Thankfully,
Hollis has not had any cravings for alcohol since she finished her program. She
is grateful for her support system, and she reaches out to them if she has any
triggers.
“They are
random, and I’m blessed because they’ve been few and far between. They’ve
usually been when I’m stressed after a long day at work,” she explained. “I
instantly reach out to either a family member or someone from group.”
Her pastor
has also been a major source of comfort through her recovery. As an ordained
minister, Hollis leans on her faith continuously. She prays daily and meditates
for about 20 minutes each morning and evening.
“That’s
what’s working for me right now.”
The goal
is helping others
April is
National Alcohol Awareness Month. For Hollis, sharing her story is scary, but
she hopes it can help others who are struggling.
“Never think
‘it can’t happen to me.’ We are all in the grips of grace. This is a disease,
and it can affect anyone and everyone who is not set up with the correct coping
skills, regardless of our education, intellect and position in life,” she said.
“Asking for help did not make me less than or weak. It actually restored my
healing and my life.”
For Villecco,
she knows that someone must be fully committed to treatment with their heart,
mind, body and soul or else it may not work for them.
“I will say
this though,” she said. “I love to plant a seed and will be there, ready to
help it grow if they are ready for change.”